Acute Myocardial Infarction (AMI)
Acute Myocardial Infarction or DAMI (Direct Admission Myocardial Infarction)
Myocardial infarction (MI), also known as a heart attack, occurs when blood flow decreases or stops to a part of the heart, causing damage to the heart muscle. The most common symptom is chest pain or discomfort which may travel into the shoulder, arm, back, neck or jaw. Often it occurs in the center or left side of the chest and lasts for more than a few minutes. The discomfort may occasionally feel like heartburn. Other symptoms may include shortness of breath, nausea, feeling faint, a cold sweat or feeling tired. About 30% of people have atypical symptoms. Women more often present without chest pain and instead have neck pain, arm pain or feel tired. Among those over 75 years old, about 5% have had an MI with little or no history of symptoms. An MI may cause heart failure, an irregular heartbeat, cardiogenic shock or cardiac arrest.
Most MIs occur due to coronary artery disease. Risk factors include high blood pressure, smoking, diabetes, lack of exercise, obesity, high blood cholesterol, poor diet and excessive alcohol intake, among others. The complete blockage of a coronary artery caused by a rupture of an atherosclerotic plaque is usually the underlying mechanism of an MI. MIs are less commonly caused by coronary artery spasms, which may be due to cocaine, significant emotional stress and extreme cold, among others. A number of tests are useful to help with diagnosis, including electrocardiograms (ECGs), blood tests and coronary angiography. An ECG, which is a recording of the heart's electrical activity, may confirm an ST elevation MI (STEMI), if ST elevation is present. Commonly used blood tests include troponin and less often creatine kinase MB.
Treatment of an MI is time-critical.[16] Aspirin is an appropriate immediate treatment for a suspected MI. Nitroglycerin or opioids may be used to help with chest pain; however, they do not improve overall outcomes. Supplemental oxygen is recommended in those with low oxygen levels or shortness of breath. In a STEMI, treatments attempt to restore blood flow to the heart and include percutaneous coronary intervention (PCI), where the arteries are pushed open and may be stented, or thrombolysis, where the blockage is removed using medications. People who have a non-ST elevation myocardial infarction (NSTEMI) are often managed with the blood thinner heparin, with the additional use of PCI in those at high risk. In people with blockages of multiple coronary arteries and diabetes, coronary artery bypass surgery (CABG) may be recommended rather than angioplasty. After an MI, lifestyle modifications, along with long term treatment with aspirin, beta blockers and statins, are typically recommended.
Signs and symptoms
Areas where pain is experienced in myocardial infarction, showing common (dark red) and less common (light red) areas on the chest and back.
Pain
Chest pain is the most common symptom of acute myocardial infarction and is often described as a sensation of tightness, pressure, or squeezing. Pain radiates most often to the left arm, but may also radiate to the lower jaw, neck, right arm, back, and upper abdomen. The pain most suggestive of an acute MI, with the highest likelihood ratio, is pain radiating to the right arm and shoulder. Similarly, chest pain similar to a previous heart attack is also suggestive. The pain associated with MI is usually diffuse, does not change with position, and lasts for more than 20 minutes. Levine's sign, in which a person localizes the chest pain by clenching one or both fists over their sternum, has classically been thought to be predictive of cardiac chest pain, although a prospective observational study showed it had a poor positive predictive value. Pain that responds to nitroglycerin does not indicate the presence or absence of a myocardial infarction.
Other symptoms
Chest pain may be accompanied by sweating, nausea or vomiting, and fainting, and these symptoms may also occur without any pain at all. In women, the most common symptoms of myocardial infarction include shortness of breath, weakness, and fatigue. Shortness of breath is a common, and sometimes the only symptom, occurring when damage to the heart limits the output of the left ventricle, with breathlessness arising either from low oxygen in the blood, or pulmonary edema. Other less common symptoms include weakness, light-headedness, palpitations, and abnormalities in heart rate or blood pressure. These symptoms are likely induced by a massive surge of catecholamines from the sympathetic nervous system, which occurs in response to pain and, where present, low blood pressure. Loss of consciousness due to inadequate blood flow to the brain and cardiogenic shock, and sudden death, frequently due to the development of ventricular fibrillation, can occur in myocardial infarctions. Cardiac arrest, and atypical symptoms such as palpitations, occur more frequently in women, the elderly, those with diabetes, in people who have just had surgery, and in critically ill patients.
"Silent" myocardial infarctions can happen without any symptoms at all. These cases can be discovered later on electrocardiograms, using blood enzyme tests, or at autopsy after a person has died. Such silent myocardial infarctions represent between 22 and 64% of all infarctions, and are more common in the elderly, in those with diabetes mellitus and after heart transplantation. In people with diabetes, differences in pain threshold, autonomic neuropathy, and psychological factors have been cited as possible explanations for the lack of symptoms. In heart transplantation, the donor heart is not fully innervated by the nervous system of the recipient.
Women
Range of myocardial infarction symptoms in women
In women, myocardial infarctions can present with different symptoms. The classic presentation of chest pain occurs in about 50% of women. Women can also commonly experience back or neck pain, indigestion, heartburn, lightheadedness, shortness of breath, fatigue, nausea, or pain in the back of the jaw. These symptoms are often overlooked or mistaken for another condition.
Diagnosis
Criteria
An acute myocardial infarction, according to current consensus, is defined by elevated cardiac biomarkers with a rising or falling trend and at least one of the following:
Symptoms relating to ischemia
Changes on an electrocardiogram (ECG), such as ST segment changes, new left bundle branch block, or Q waves
Changes in the motion of the heart wall on imaging
Demonstration of a thrombus on angiogram or at autopsy.
Types
See also: Electrocardiography in myocardial infarction
Myocardial infarctions are generally clinically classified into ST elevation MI (STEMI) and non-ST elevation MI (NSTEMI). These are based on changes to an ECG. STEMIs make up about 25 – 40% of myocardial infarctions. A more explicit classification system, based on international consensus in 2012, also exists. This classifies myocardial infarctions into five types:
Spontaneous MI related to plaque erosion and/or rupture, fissuring, or dissection
MI related to ischemia, such as from increased oxygen demand or decreased supply, e.g. coronary artery spasm, coronary embolism, anemia, arrhythmias, high blood pressure or low blood pressure
Sudden unexpected cardiac death, including cardiac arrest, where symptoms may suggest MI, an ECG may be taken with suggestive changes, or a blood clot is found in a coronary artery by angiography and/or at autopsy, but where blood samples could not be obtained, or at a time before the appearance of cardiac biomarkers in the blood
Associated with coronary angioplasty or stents
Associated with percutaneous coronary intervention (PCI)
Associated with stent thrombosis as documented by angiography or at autopsy
Associated with CABG
Associated with spontaneous coronary artery dissection in young, fit women
Management
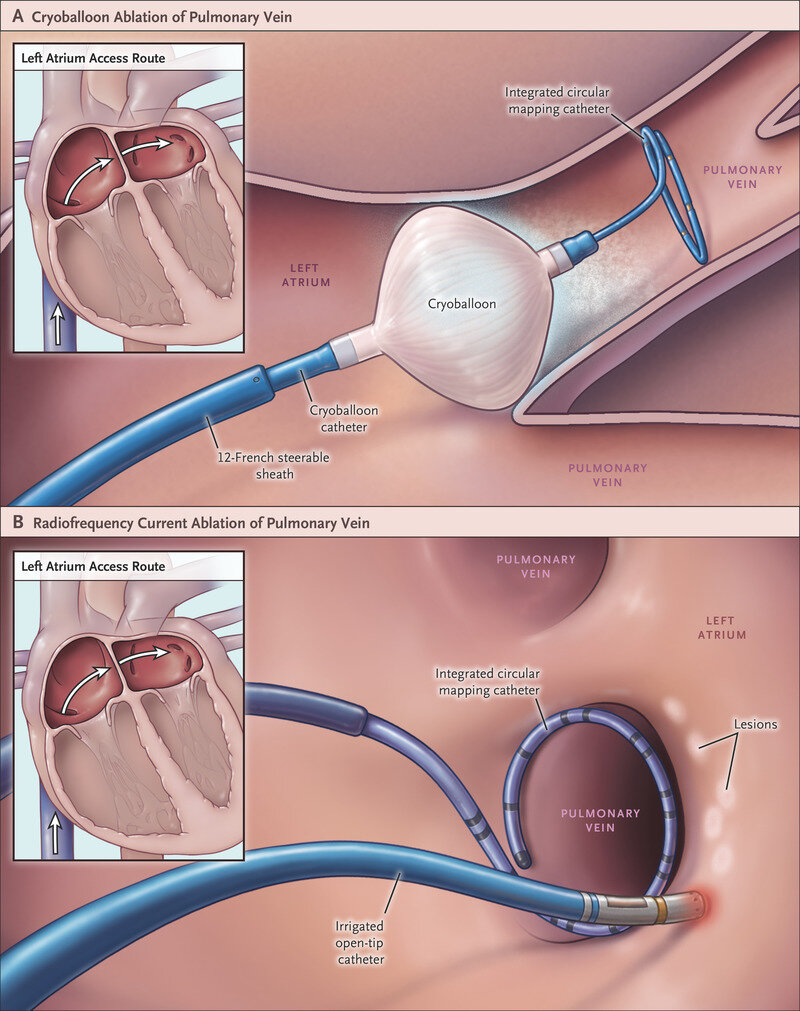
PCI (Percutaneous Coronary Intervention) to treat Acute MI
A myocardial infarction requires immediate medical attention. Treatment aims to preserve as much heart muscle as possible, and to prevent further complications. Treatment depends on whether the myocardial infarction is a STEMI or NSTEMI. Treatment in general aims to unblock blood vessels, reduce blot clot enlargement, reduce ischemia, and modify risk factors with the aim of preventing future MIs. In addition, the main treatment for myocardial infarctions with ECG evidence of ST elevation (STEMI) include thrombolysis or percutaneous coronary intervention, although PCI is also ideally conducted within 1–3 days for NSTEMI. In addition to clinical judgement, risk stratification may be used to guide treatment, such as with the TIMI and GRACE scoring systems.
EQUIPMENT FOR HAC NURSE and CATHLAB STAFF:
Guidecatheters: (For HAC nurse to prepare) *Heart Attack Centre (HAC) Nurse
LCA (for left coronaries) (usually if anterior and lateral ST elevation) *See images below
- 6F EBU 3.5 guidecatheter
6F JR4 diagnostic catheter
RCA (for right coronaries) (usually if inferior and posterior ST elevation) *See images below
- 6F JR4 guidecatheter catheter
6F JL3.5 diagnostic catheter
SEDATION: (Managed by Circulating Nurse)
Midazolam 2mg/2mL (give in 0.5mg increments)
PAIN RELIEF:
Morphine 10mg/2mL (give in 2.5mg increments)
For IV drug line
- 500 mL saline bag
- Extension line (long)
- 3-way tap
- 20mL luerlock syringe
- 2ml or 5 ml luerlock syringe (labeled, for midazolam)
- blunt needle for aspirating drugs
- giving set
Supplies: (prepared by scrub nurse)
- ANGIO-pack (KIMAL)
- Spike for saline bag
- 2 chloraprep
- 500ml NSS (sterile bag)
- Tegaderm dressing (to secure radial sheath)
- 6F Terumo radial sheath (Radial Approach) or 6F Cordis femoral sheath (Femoral approach)
- Inflator device
-short hemostasis valve extension
-Contrast balloon mixture (50mL contrast: 50mL Saline)
-30mL luerlock syringe
-Angioplasty wire (operator preference) or ASAHI Sion Blue (commonly used workhorse wire)
-Angioplasty balloon (size depending on the vessel diameter)
-Semi-compliant (for predilation)
-Non-Compliant (for postdilation)
-Drug-eluting stent (size depending on the vessel diameter)
Medications (prepared by Scrub Nurse):
- Lidocaine 1% 5ml amp if radial (20ml if femoral)
- Heparin 10,000iu/10mL
- 1 amp Isosorbide Dinitrate 10mg/10ml (Dilution: ISDN 2mg/2mL add with 8mL NSS to make 2mg/10mL or 200mcg/mL dilution)
- 1 amp Verapamil 2.5mg/2ml (Dilution: Verapamil 2.5mg/mL add with 4mL NSS to make 2.5mg/5mL)
Closure devices:
- Angioseal (6F or 8F) if femoral access
- TR band or Helix (regular or large) if radial access
PROCEDURE STEPS
if RADIAL APPROACH:
Operator injects 2-3 mL of Lidociane 1% subcutaneously
Inserts the sheath using Seldinger Technique
Aspirates blood from sheath to confirm patency of the puncture
Verapamil 2.5mg/5mL through the sheath (spasm prevention)
Then introduce catheter with guidewire (JR4 first for RRA, JL4 for RFA)
Introduction of Angioplasty wire (usually Sion Blue) and park the wire distal to the coronary lesion
Predilation of the lesion with Semi-compliant balloon
Deployment of coronary stent
Post-dilation with Non-Compliant (NC) balloon, if necessary
Closure of radial/femoral access.
STANDARD VIEWS for Coronary Angiography
For RCA:
LAO 30
LAO 20 CRAN 20 / PA CRAN 30
RAO 30
For LCA:
PA CAUDAL 40
LAO 40 CAUDAL 40
LAO 10 CRAN 40
RAO 40 CRAN 40
RAO 30 CAUD 30
Photos and Diagram
Items to be added to Angio Pack (prepared by Scrub Nurse)
Items for IV DRUG LINE (Prepared by HAC Nurse or Running Nurse)
Guidecatheter (EBU3.5) and Diagnostic Catheter (JR4) to prepare, if with ANTERIOR or LATERAL ST Elevation on ECG
Guidecather (JR4) and Diagnostic catheter (JL3.5) to prepare, if with INFERIOR ST Elevation on ECG
Standard step of Coronary Angioplasty and Stenting
Sizes of Semi-Compliant Balloons
Different sizes of Coronary stents
Non-Compliant balloons
Medications the scrub nurse will need
If there’s a suspected thrombus or clot formation in the coronaries